Is Gastric Sleeve effective?
Gastric Sleeve Surgery is a remarkable tool to reduce Body Mass Index (BMI) and improve overall metabolic health. Surgery on its own is not a magic wand, but when paired with a supportive lifestyle and behavioural modifications, losing excess weight and, importantly, keeping it off is a genuine possibility.
This Bariatric Surgery is gaining popularity because it helps patients achieve good results. The Gastric Sleeve success rate is between 80% and 90%. On average, people who undergo this Weight Loss Surgery lose 60-70% of their excess weight within one year.
How does Gastric Sleeve help you lose weight
Gastric Sleeve Surgery changes on three levels: metabolic change, restriction and malabsorption. By removing about 70% of the stomach or fundus, the surgery alters and stabilises “hunger hormones” and helps patients feel more satisfied. The surgery reduced the volume of food consumed quite significantly while providing a level of malabsorption of some calories and specific nutrients.
Reduced hunger, better hormonal regulation, decreased intake, and limited absorption helps the patient lose weight. Average weight loss with Gastric Sleeve is approximately 60-70% of excess weight in the first year. Maintaining the loss with healthy food and lifestyle choices is essential to keep the weight off and improve metabolic health overall.
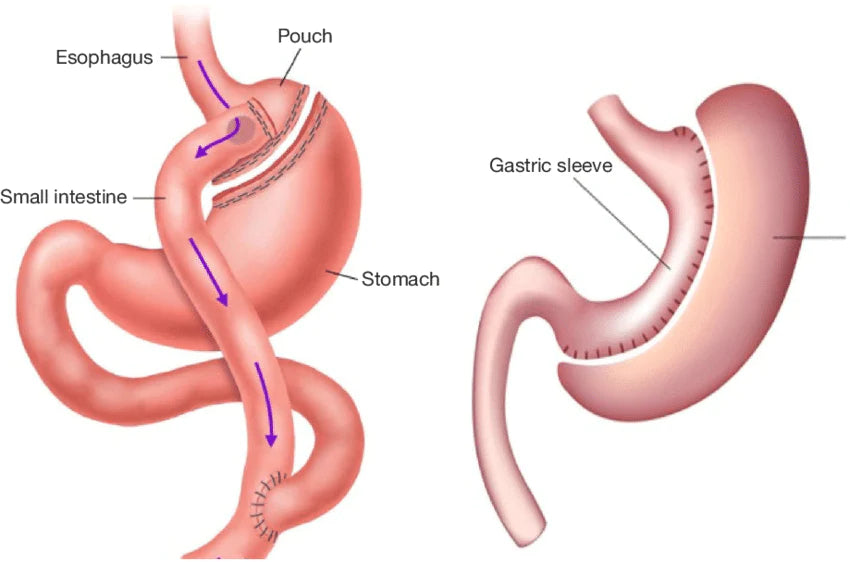
Comparison to Other Bariatric Procedures
When comparing the various Bariatric Surgeries, it's important to consider that your doctor will recommend the amount of weight you have to lose and your overall safety based on your unique situation.
When drawing comparisons,Gastric Sleeve V Gastric Bypass has pros and cons.
- Both have the same objectives: Reduced BMI, improved health and metabolic status.
- Gastric Sleeve is irreversible, Gastric Bypass is reversible, but it is a complex procedure only used in very unique situations
- Gastric Bypass has been shown to produce greater weight loss, but more significant restriction and malabsorption come with that.
So whilst the risk of nutritional deficiency is apparent with the Gastric Sleeve, there is a greater risk and a broader range of nutrients affected by the Bypass surgery.
Who is a good candidate for this surgery?
Any type of surgery comes with its own set of risks and benefits. The qualifications for Gastric Sleeve Surgery at the time of writing are as follows: BMI of at least 40 or should have a BMI of at least 30 AND have at least one obesity-related severe, co-morbid health condition. Your doctor will work with you on deciding if you qualify and will also be instrumental in advising on the safest and most effective scenario for your situation.
Step by Step Surgical Procedure
The Sleeve Gastrectomy is carried out laparoscopically or via keyhole surgery. The surgeon will follow a step by step surgical procedure that includes using cameras and other surgical equipment inserted through “ports” in the patient’s abdomen.
The process carefully removes part of the stomach, stitching up the new sleeve.
Gastric Sleeve Procedure
The Gastric Sleeve Surgery procedure generally takes one to two hours to complete. The following steps after the Gastric Sleeve procedure are the beginnings of the recovery period. During the time needed for healing and metabolic changes to occur, a step by step introduction back to solid foods is done very carefully.
The initial phase after the operation is a liquids phase where only nourishment is obtained through liquids. The liquid stage is followed by a puree stage where a smooth “baby food” consistency is adhered to.
Finally, a progression to soft and solid foods, to eat a well balanced healthy diet to make the most out of the new “tool” and encourage permanent weight loss.

Pre-Op Lifestyle Changes
In the lead-up to Bariatric Surgery, the "pre-op stage” is the preparation for a new lifestyle change, the mindset is beginning to be addressed, and the safety of the surgery is front of mind. The pre-op diet is generally prescribed two weeks before the surgery date, encompassing a very low calorie and carbohydrate, higher protein diet - using meal replacement shakes or healthy food.
Most patients who qualify for WLS have an enlarged liver, leading to complications during the surgical procedure. The pre-op diet is directly aimed at reducing the size of the liver to ensure the patient's safety. Regular exercise and other crucial pre-op lifestyle changes like giving up alcohol and smoking will be discussed at this stage also.
Pre-Surgery Diet
The Gastric Sleeve pre-op diet is critical to the surgery's success in reducing your liver's size, which improves surgical access to the stomach.
In many cases, you should begin your Gastric Sleeve pre-surgery preparation three weeks before your procedure. You will usually plan your meals to:
- Reduce calories – especially carbohydrates
- Maximise protein intake
- Focus on healthy fats
- Drink plenty of water
You'll follow a pre-op liquid diet for Gastric Sleeve between 2-3 days before surgery. Please talk to your bariatric team for more details on when to start your diet. Failure to follow these guidelines may jeopardise your eligibility for the Gastric Sleeve procedure.
What happens during Gastric Sleeve Surgery?
The surgery itself is a fairly straightforward process; the laparoscopic Gastric Sleeve uses 5-6 ports or incisions made in the abdomen to insert surgical equipment and a camera.
The surgeon can first see that the environment is safe to operate in and that the procedure is precise. The overall outcome is removing approximately 70-80% of the existing stomach or fundus and subsequent stapling together the remaining tissue to form the new stomach or sleeve. New technologies are developing in the realm of Bariatric Surgery, and a minimally invasive or single-incision Gastric Sleeve procedure is available, where all the work is done via one incision in the umbilicus or belly button.
Life after Gastric Sleeve Surgery
Many prospective patients are keen to hear about life after Gastric Sleeve Surgery. Its often met with a range of feelings from relief - finally finding a solution that actually provides sustainable weight loss and improvements in metabolic health, to overwhelm and confusion around just how much there is to learn about self-care, behaviour and nutrition to make the best use of this new tool provided by the surgery.
Gastric Sleeve post-op recovery is carefully monitored for complications, and a graduated return to eating solid foods is prescribed to ensure the patient's safety while the surgical sites heal and the body adjusts to its new formation.
Overall, with the ongoing support of a multi-faceted professional team including a dietitian, psychologist, exercise physiologist and GP, many patients find their way along the path to weight loss success and recession of the health impacts of having a high BMI.
Why is it important to prepare for recovery?
Gastric Sleeve recovery time is generally six weeks of dietary limitations such as the liquid and puree stage. Its recommendation is to rest when needed and abstain from physical activity or lifting for some time- overall focus on meeting the dietary recommendations for protein and nutrients by using a Bariatric Multivitamin supplement to make up for the limited range of food and nutrients.
Preparing for recovery by being healthy and nutritionally sound in the lead up to surgery will reduce the risk of complications by a large degree.
What is recovery after the surgery like?
Recovery from Gastric Sleeve Surgery can range from a dream run of mild pain, some gas pain and incision site pain and bruising to dehydration, weakness, vomiting and intolerance to some foods and liquids.
Overall, the Gastric Sleeve recovery time is a period of trial and error and persistence. The best approach to recovery is to be as well educated as possible by researching the process well before surgery.
A good start is to have implemented some of the necessary lifestyle changes even before the WLS journey begins.

What can you expect during your short-term recovery?
The focus of the short term recovery or the amount of time spent in the hospital will generally be reliant on a few factors:
- Hydration: In the hospital, a hydration goal is provided, and release can be quite dependent on the ability to sip sip sip.
- Movement: Helps mitigate gas pain and is also essential for preventing blood clots.
- Pain Management: Having pain well-controlled will speed the recovery process; Research has shown that unmanaged pain slows the healing process.
- Lack of complications: The team will monitor any post-surgical complications signs before being released from the hospital.
Post-Surgery Diet
The Gastric Sleeve post-op diet is graduation from liquids back to solid foods - much like the guide for eating foods after Gastric Bypass.

Liquid diet after Gastric Sleeve
Meal replacements, smoothies, broths and other clear liquids for the first few weeks.

Puree stage
Healthy protein-rich foods pureed to a consistency of baby food, with no large lumps. Most foods can be blended to this consistency, and if not loose enough, some added water or other liquid can be added.

Soft food stage
Slow cooked meats and vegetables, soft scrambled eggs, frittata, and stewed fruits are great healthy options for this stage.
Then the aim of the post Gastric Sleeve diet long-term is to move to a solid and varied diet aimed at weight loss.
Portion management bowls and plates are an essential tool, and excellent awareness of the protein content of the foods and drinks eaten will help ensure that all critical protein targets are reached.
Bariatric Multivitamins are a crucial part of the post-surgery diet and are also recommended for life after Bariatric Surgery.

Exercise after Surgery
Once the initial recovery period is over, and the surgeon has approved, exercise is recommended as part of the healthy lifestyle that is important to adhere to for a successful outcome after Gastric Sleeve.
Exercise after Gastric Sleeve depends on a few critical factors:
Long-Term Expected Results
A Sleeve Gastrectomy is an effective tool for assisting with excess weight and health complications related to obesity. The long term effect of a Gastric Sleeve on the loss of excess weight averages about 60-65% (excess weight = the proportion of weight above the healthy weight range).
- Up to a quarter of patients may require a second surgery to achieve this weight loss or treat reflux over ten years.
- Studies show fewer heart attacks and other cardiac events.
- For type II diabetics, Sleeve Gastrectomy is influential in improving control or providing remission from diabetes. More potent than drug treatment alone.

Essential Tools for Long-Term Success
The surgery is an excellent tool for reducing portion sizes and making the metabolic changes needed to support weight loss. The first 12-18 months are critical for reviewing behaviours around food, establishing portion control, maintaining a higher protein diet, removing refined carbohydrates, and adding fresh foods.
Careful monitoring of food behaviours and “habits” is critical. These will start to make their way back into the diet around the 12-18 month mark and must be managed carefully to avoid weight regain and malnutrition.
Long-term, the most successful patients, do the work. They are proactive and responsible for their health and habits, consistently engage with their support team, and reach out if they notice something is changing or struggling.
Commit to taking your Bariatric Multivitamins every day for life to manage the malabsorption and malnutrition brought about by your surgery.
Advantages and Disadvantages of Gastric Sleeve Surgery
Gastric Sleeve Surgery carries certain advantages and possible disadvantages.
Nutritional Risks and Side Effects after Gastric Sleeve
Before surgery, most obese patients already present many nutritional deficits. These findings prompt a complete dietary assessment and an adequate correction of pre-existing deficiencies. Thereby potentially decreasing any nutritional deficiencies during surgery.
Gastric Sleeve Surgery alters the digestive tract, which impacts dietary intake and nutrient absorption, namely, deficiencies of macro and micro-nutrients, which could lead to enabling risks such as anemia, osteoporosis, and protein malnutrition. Many of these risks can occur when you take in fewer nutrients and do not follow the Bariatric team's guidelines.
You can prevent nutritional complications after Gastric Sleeve by lifelong nutritional monitoring and supplementing with specific Bariatric multivitamins and supplements according to the patient's needs. This can really impact how you feel and how you recover.
It is crucial to have regular blood tests to detect and treat nutritional deficiencies. Your Bariatric surgeon will detail all potential risks with you during your initial consultation.
Gastric Sleeve Surgery Frequently Asked Questions
-
How long does Gastric Sleeve Surgery take?
Generally, Gastric Sleeve Surgery takes around 1-2 hours to complete and is performed laparoscopically and under general anesthesia. You may need to remain in the hospital for 1-3 days following surgery.
-
Is the Gastric Sleeve covered by insurance?
We advise all patients considering Gastric Sleeve Surgery to check that they have an appropriate level of cover for their private health insurance. Not all private health insurance covers bariatric surgeries. To determine if your insurance covers Gastric Sleeve Surgery, simply call your private health insurer and quote the surgical item number for the Gastric Sleeve (31575).
-
Cost of Gastric Sleeve Surgery without insurance
Gastric Sleeve Surgery is not generally available in the public hospital system. Without health insurance, your surgery must be funded through the private hospital system. Without insurance, Gastric Sleeve Surgery can be around $20,000*, including fees for your surgeons, dietitians, anaesthetist, operating theatre, and hospital stays.
*This is an estimated cost only and may vary depending on your situation.
-
How much do you have to weigh for a Gastric Sleeve?
If you are considering Gastric Sleeve Surgery; you should have a BMI of at least 40 (usually translates to being overweight by 45.4 kgs or more) OR have a BMI of at least 30 AND have at least one severe obesity-related health condition.
-
How much weight do you lose with the Gastric Sleeve?
You will generally result in 25-35% body weight loss OR 50-70% excess weight loss with Gastric Sleeve Surgery from your starting point1. Your excess body weight is the difference between your current and ideal weight. Some can lose less, while others lose more than 70% of their excess weight. You also have to consider determining whether you are changing your dietary behaviours, lifestyle, and exercise regime after surgery.
-
How much protein do you need after Gastric Sleeve Surgery?
Depending on your situation, most bariatric surgery programs will recommend 60-100 grams of protein intake daily2. Therefore, eating high protein foods from animal sources (beef, chicken, turkey). Patients who do not consume enough protein can cause severe problems and experience muscle loss and weakness.
-
How much can I eat after Gastric Sleeve Surgery?
Bariatric diet recommendations after Gastric Sleeve Surgery will vary depending on your situation. Typically, you'll follow three stages of eating before aiming for observing a regular nourishing range of foods. Each stage will help you receive all the nutrients you need for your digestive system to heal and recover from surgery. How promptly you move from one stage to the next depends on how fast your body recovers and adjusts to changing eating patterns.
Click 'Post-Surgery Diet' to see more about the methods that need to be applied to eating for life after Gastric Sleeve Surgery.
-
Certain tests before approval for Gastric Sleeve Surgery are:
A complete blood count
Urinalysis
Chemistry panel: Provides around 20 blood chemistry values
Gallbladder ultrasound: Look for gallstonesOther tests may be required when indicated:
Cardiology evaluation
Psychiatric evaluation
GI evaluation
Chest X-ray
Electrocardiogram
Pulmonary function testing
Echocardiogram
Sleep studies -
Pre-op testing for Gastric Sleeve:
An accurate assessment of your health is required before your Gastric Sleeve Surgery to prevent complications and understand any potential complications that could arise. The pre-op testing for Gastric Sleeve will determine if you have:
- Breathing difficulties
- Liver malfunction
- Abnormal blood fat levels
- Excess fluid in the tissues
- Abnormalities of the salts or minerals in body fluids